Member Blog


Spring into action! Learn how to build a lasting exercise habit with our 4-step guide: identify your "why," set a specific plan, and overcome common barriers
Read the article
Recipes you might like
Thank you! Your submission has been received!
Oops! Something went wrong while submitting the form.


12 Foods That Are Bad for Your Heart and What to Eat Instead for Heart Health Month
February 24, 2026
/
8
min
Cardiometabolic Management
Cholesterol
Whole grain
fiber
Healthy Lifestyle


Heart Health Month: Understanding Your Lipid Panel and How to Improve Cholesterol and Triglycerides
February 17, 2026
/
8
min
Cholesterol
Cardiometabolic Management
Heart Health
Hypertension
Healthy Lifestyle


Understanding Your ASCVD Risk Score: Tips for Heart Health Month
February 10, 2026
/
9
min
Cardiometabolic Management
Heart Health
Nutrition
Cholesterol
Diabetes


Your Game Day Plan: Winning Plays for Weight Loss at the Football Championship
February 2, 2026
/
10
min
vegetables
Side
beverage
Blood Sugar
Weight Loss


Re-Set Your Goals: 20 Tiny Steps for Better Nutrition
January 27, 2026
/
min
holidays
Diet & Exercise
Weight Loss
Nutrition
Prediabetes


Overcoming Exercise Barriers: How to Stay Active
January 20, 2026
/
7
min
Exercise
Blood Sugar
Healthy Lifestyle


10 Identity Shifts for the New Year to Help You Be the Healthy Person You Want to Be
January 13, 2026
/
8
min
holidays
Diet & Exercise
Healthy Lifestyle
Weight Loss


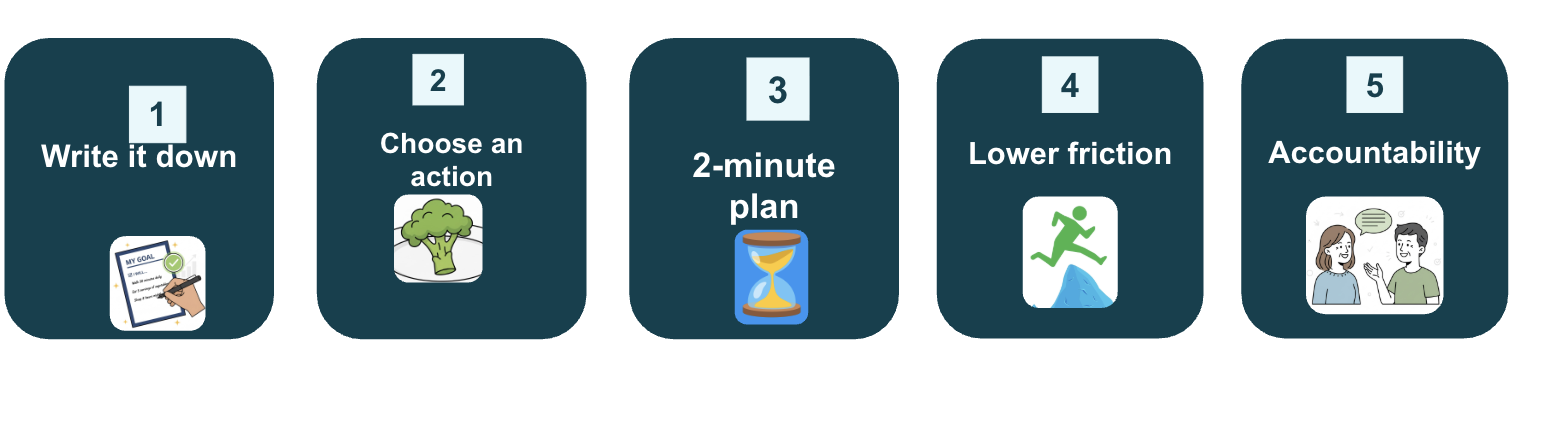
A Simple 5-Week Plan to Build Healthy Habits to Achieve Your New Year’s Goals
January 6, 2026
/
min
Recipes
Healthy Lifestyle
Blood Sugar
Weight Loss
Diet & Exercise
-images-0.jpg)
Lark Stop Wishing, Start Doing Worksheet
January 1, 2026
/
min
Weight Loss
Healthy Lifestyle
Prediabetes
GLP-1


Reflecting on the Old Year to Prepare for the New
December 30, 2025
/
min
Prediabetes
Healthy Lifestyle
Diet & Exercise
Weight Loss


Your GLP-1 Holiday Guide: How to Thrive (Not Just Survive) This Season
December 23, 2025
/
11
min
holidays
GLP-1
Medication
Foods
Diabetes


10 Must-Have Items for Your Healthier, More Joyful Holiday Table
December 16, 2025
/
10
min
holidays
Protein
Weight Loss
Healthy Lifestyle


