Imagine it’s 7:13 PM. A member with pre-diabetes and hypertension is out for dinner to celebrate a recent promotion with friends. She thinks she knows the right choices to make, but isn’t sure— her next doctor’s appointment is three weeks away and she’s trying to make healthy choices. She’s on her own.
At the same time, another member who recently started GLP-1s is struggling to take his medication consistently and determine the right diet and activity to build new habits. He feels stuck and is waiting for his next doctor’s appointment in a month to determine what he should be doing differently.
Moments like this happen thousands of times a day to members - and rarely happen in the doctor’s office.
That’s the problem.
If we want to improve health outcomes and rein in costs, we have to rethink how we support members' cardiometabolic health. Instead of focusing on appointments, let's design solutions that fit into their daily lives.
Life Doesn’t Happen on a Schedule. Neither Should Cardiometabolic Support.
Traditional healthcare is primarily built around episodic treatment, focusing on symptoms, diagnosis, and follow-up appointments. But managing conditions like obesity, diabetes, cholesterol, and hypertension isn’t intermittent and requires daily vigilance to improve conditions.
Between appointments, a person's daily habits—like what they eat, how they sleep, and how they manage stress and exercise—have a bigger impact on their health than any single doctor's visit. However, most healthcare models provide little support for in these moments.
This gap comes at a cost for everyone.
Fragmented care has been associated with an increase in adverse events, including coronary heart failure and severe risk of infection. These events can have a devastating impact on patients and increase health care costs by 75% for extreme cases. Delayed intervention leads to worse outcomes, higher med utilization, and unnecessary ER visits.
Members often feel disconnected from their health journey when care is not connected, and this can lead to disengagement and frustration. It’s no surprise that 69% of large employers say they’re concerned about siloed care experiences.
What Members Want (and Need) Is Access to Support In the Moments that Matter
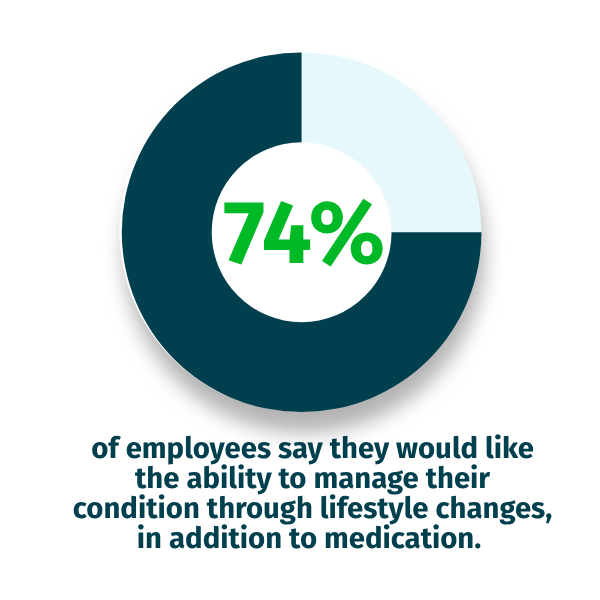
A vast majority of employees with chronic conditions (80%) are already on medication and looking for better ways to manage their health. Seventy-four percent of employees say they would like the ability to manage their condition through lifestyle changes, in addition to medication.
Solutions that offer access to daily coaching, education, and support for medication adherence see greater member engagement and measurable health improvements. Digital tools rooted in behavioral science, such as Cognitive Behavioral Therapy (CBT), have been proven to help build sustainable habits that drive positive outcomes.
Simply adding more care options isn't what helps members. What they need is timely, personalized support that fits into their daily lives.
Digital Coaching Requires A Blended Approach for Success
During your selection process, it is essential to understand how chronic care programs tailor their support to each member’s unique needs, ensuring you deliver useful and relevant support.
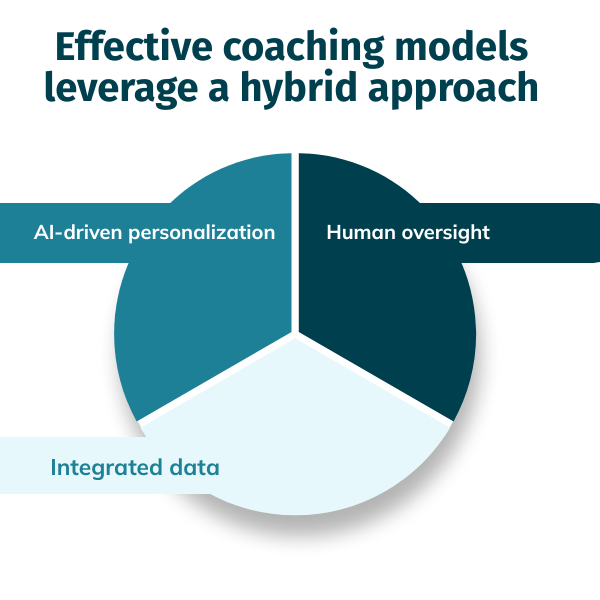
The most effective coaching models are powered by a hybrid approach:
- AI-driven personalization delivers timely nudges, content, and encouragement based on real-time behavior and preferences, adapting to each member’s unique journey.
- Human oversight ensures members can escalate to a coach or integrated clinician of their choice when needed.
- Integrated data from wearables, logs, and devices provides a comprehensive picture of each member’s health journey, offering accurate and timely insights.
Deploying AI-powered health technology within your benefits strategy should never replace care, but it can help scale support for members to better manage their conditions in moments when traditional options are not available. Technology woven into the benefits strategy helps every member feel seen, supported, and empowered in the moments that matter.
Why It Matters for 2026 (And Beyond)
The stakes are only getting higher. GLP-1 demand is growing and costs are soaring as a result; however, without support to drive behavior changes, outcomes are mixed.
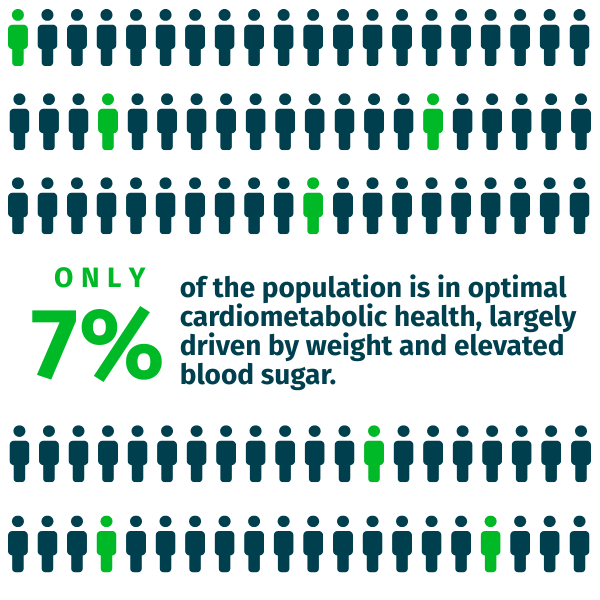
The impact of cardiometabolic conditions is becoming a growing concern, with only 7% of the population in optimal cardiometabolic health, largely driven by weight and elevated blood sugar. Employees are seeking support that integrates seamlessly into their day-to-day lives and delivers effective results.
HR and benefits leaders can’t afford to wait for another cycle of fragmented care. In 2026, we must move beyond appointment-based models and build something better: care that’s continuous, compassionate, and clinically sound.
If you want to empower members to improve outcomes and reduce your benefits, your benefits model has to extend beyond the four walls of doctors’ offices and rigid business hours. It has to follow your members into their homes, their routines, and their daily decisions.
That means:
- Prioritizing vendors who offer 24/7 digital coaching that scales across your entire population
- Ensuring wraparound support for GLP-1s and chronic conditions
- Making every touchpoint feel personal, proactive, and always within reach
Because healthcare doesn’t stop when the office closes. And neither should your benefits strategy.
Looking to integrate 24/7 coaching into your 2026 benefits plan? Contact Lark to discover how our programs deliver effective and scalable results.




.jpeg)






.webp)



.png)

.jpg)